What is Stress Urinary Incontinence?
Stress Urinary Incontinence (SUI) occurs when urine leaks during exercise, coughing, sneezing, laughing or any movement that puts pressure (stress) on the bladder.
How does Stress Urinary Incontinence affect the bladder?
Not all women will experience SUI in the same way. Some women will only leak when they exercise vigorously or when they have a full bladder. Other women, however, may experience bladder leakage from daily living activities, such as walking or sneezing. While the amount of urine leakage may differ, at some point SUI may interfere with your activities, intrude on your social life, or be just plain inconvenient and embarrassing.
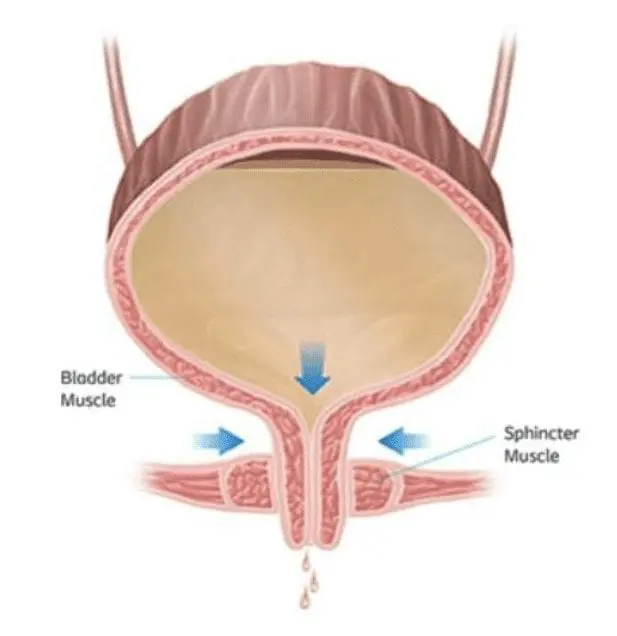
- Bladder leakage in SUI is due to the weakening of the pelvic muscles and tissue that normally support the bladder.
- In a standard functioning bladder, the muscles in your urethra stay closed to prevent urine from escaping the bladder until you have reached the bathroom.
- With SUI, however, any force that is exerted on the bladder through physical movement such as running, sneezing or laughing, may cause your bladder to leak since weakened pelvic muscles are no longer staying closed.
Causes of Stress Urinary Incontinence
Stress urinary incontinence can develop slowly as you age or may be a result of a specific event or factors.

Risk factors include:
- Childbirth
- Previous pelvic surgery
- Menopause
- Obesity
Other conditions linked to stress urinary incontinence include depression, urinary tract infections, smoking, and diabetes. It can also occur with repetitive straining such as chronic coughing or high-impact activities such as aerobics and running.
Tests for Stress Urinary Incontinence
How is urinary incontinence diagnosed?
As there are many different types of urinary incontinence which share the same symptoms, it is important to get an accurate diagnosis to ensure that the appropriate treatment is selected. The first step is to seek out a physician that specializes in Pelvic Floor Disorders such as urogyns as they have received special training to diagnose and treat women with urinary incontinence.
Medical History
The first thing your physician will ask is for a complete rundown on your medical history, which includes any medication or supplements you may be taking. Next, your physician will want to know about your bladder leakage symptoms and when you experience them. Being as truthful as possible is important. It is easy to become embarrassed or uncomfortable, but accurately describing your symptoms is the first step to finding a solution.
Physical Exam
After you have discussed your medical history, a physical exam will often be conducted. Your specialist may look to see if you have any additional pelvic floor disorders that may be related to your bladder leakage. Next, your physician may ask you to do a “cough test” to see how well your bladder holds up to stress during normal daily activities. Your physician could also ask you to do an “at home pad test”. This test will help to estimate how much you are leaking throughout the day to determine the severity of your urinary incontinence. There are bladder imaging and bladder function tests that can also be conducted if your physician needs additional information to diagnose your symptoms accurately.
Symptom Checker
Do you show symptoms that could identify stress urinary incontinence? Read the bullets below and ask yourself if you leak during any of the activities. If you say yes to one or more, you may have symptoms of stress incontinence and should consult with your doctor.

Do you leak urine during the following activities?
- Laughing
- Coughing
- Sneezing
- Heavy Lifting
- Physical Activity
- During Intercourse
Remember, although these signs and symptoms can alert you to a problem, they are not unique to stress incontinence, so it is important to consult a doctor for the correct diagnosis.
Treatment Options for Stress Urinary Incontinence
Non-surgical Treatment Options
pads and protective undergarments
When women first start to experience bladder leakage, often the first option they look at is liners or pads.
Many women feel they can manage their day-to-day bladder leakage with liners, pads, disposable or reusable underwear. While pads do provide some degree of protection and discreet management, they do not try to improve your bladder function, unlike other treatment options.
lifestyle changes
Before or in conjunction with other treatment options, a specialist will often suggest lifestyle changes to help decrease bladder leakage:
- Lose Weight: Carrying extra weight can have an impact on bladder leakage. You may benefit from losing even a small amount of weight.
- Manage Your Fluid Intake: If you find that you experience bladder leakage at night or in the morning, reducing the amount of liquid before bed could help. Limiting caffeine and alcohol can also be beneficial.
pelvic floor muscle exercises and biofeedback
Bladder leakage in stress urinary incontinence is most often due to the weakening of the pelvic muscles and tissue that normally support the bladder, actively strengthening the pelvic muscles may help lessen your symptoms.
- Physical Therapy: Going to see a pelvic floor provide guidance on a treatment plan to help you regain pelvic floor function.
- Kegels: Kegels are an exercise you can do on your own to help strengthen your pelvic muscles.
- Biofeedback: As pelvic muscles are hidden from view; it can be hard to determine if you are doing Kegels correctly. Biofeedback can be used to offer real-time feedback to show when you have targeted the correct muscles during physical therapy exercises, such as Kegels.
pessary
A pessary is a small plastic device that is inserted into the vagina to help support the vaginal walls and provide lift to the bladder and urethra. Pessaries are available in a variety of sizes. Your provider will provide instructions on inserting and removing the device. To ensure you receive a pessary that is fitted correctly, it’s important to see a specialist who can provide guidance on what size is right for your body.
medication
While there are [prescription] medications that can help reduce the symptoms of bladder leakage, medication currently only treats urge urinary Incontinence and overactive bladder. If you are suffering from mixed urinary incontinence (a combination of stress and urge incontinence), you may benefit from using medication for urge incontinence. However, you may need additional treatments to decrease bladder leakage related to stress urinary incontinence.
Surgical Treatment Options
If non-surgical options have not solved your stress urinary incontinence, it may be time to consider a more permanent surgical solution. One surgical option your doctor may recommend is a sling procedure.
A sling procedure corrects stress urinary incontinence by supporting your urethra to keep it in its correct position. The operation is a minimally invasive outpatient surgery. A sling corrects bladder leakage, or stress incontinence, by providing support to the bladder neck and urethra. After a sling procedure, most women can regain better control of their bladder. It is important to know that future pregnancies may negate the effects of the surgical sling procedure and you may once again become incontinent.
There are different types of sling procedures, including a Transobturator, a Suprapubic, a Retropublic and a Single Incision – each of which implants the device using a different method or approach. Your doctor will discuss the differences and which type of procedure might be best for you.
Frequently Asked Questions
We’ve compiled some of the most common questions that women ask when learning about stress urinary incontinence. Read for yourself to learn more about stress urinary incontinence causes, symptoms and treatment options.
What is urinary incontinence?
Urinary incontinence is the loss of voluntary control over your urinary functions. Approximately 18 million women in the U.S. suffer from urinary incontinence. That’s 1 in 4 women over the age of 18.
Are there different types of urinary incontinence?
Yes. The most common types are stress, urge and mixed, which is a combination of the two. Stress incontinence happens when urine leaks during coughing, laughing or exercise because the urethra does not function properly. Urge incontinence involves the sudden sensation of the need to urinate that can be hard to put off – the sudden urge to go. Mixed is a combination of stress and urge incontinence.
What causes female stress urinary incontinence?
Female stress incontinence generally occurs when your pelvic muscles are not strong enough to keep the opening of the bladder neck closed when there’s pressure on your bladder from laughing, coughing, lifting, exercising or other activities that cause abdominal pressure. It can slowly develop as you age and may be the result of a specific event such as childbirth, or be a result of smoking, obesity or other previous tissue traumas in the area.
Can stress urinary incontinence be successfully treated?
Yes, stress urinary incontinence can frequently be treated with women seeing their symptoms improve.4 It is quite common for life events like childbirth or menopause to contribute to bladder leakage, but that does not mean that bladder leakage is considered normal at any age. There are many different treatment options available for stress urinary incontinence. It is important to discuss the problem with your doctor to find out what treatment may be right for you.
What are the treatment options for stress urinary incontinence?
Treatment options for stress urinary incontinence range from the day-to-day management of symptoms to surgical treatments that provide a permanent solution.6 Examples of non-surgical options include wearing pads or absorbent undergarments or improving pelvic strength through muscle exercises. Surgical treatments include stress incontinence surgery that utilizes either your own tissue or a synthetic sling to support the urethra to help you regain bladder control. Your doctor can discuss these options to determine the best choice for you.
What is a stress incontinence surgery?
Stress incontinence surgery may be approached in different ways. In some cases, the surgeon may use your own tissue to correct your incontinence. Another minimally invasive6 option uses a synthetic or biologic material to help support your urethra, which is commonly known as a “sling.” It helps cradle the urethra by providing additional support to help correct urinary incontinence.
What can I expect after stress urinary incontinence surgery?
In a recent study, 113 women had the Altis® sling implanted, and after two years 90.4% of women state they are “much better or “very much better,” 87.9% did not leak after they coughed during a test (a “cough stress test”).
Can I become incontinent again after having a stress incontinence surgery?
It is possible to become incontinent after stress incontinence surgery. One factor to consider is that future pregnancies following stress incontinence surgery may negate the effects of your surgery and you may once again become incontinent.
How long does it take to recover from a stress incontinence surgery?
Every patient’s recovery time is different following surgery. During your recovery, be sure to avoid heavy lifting and sexual intercourse for six weeks or as recommended by your doctor. Your doctor will provide you with specific details about your recovery process.
What are the risks associated with stress incontinence surgery?
Some of the more common side effects from surgery include: mesh erosion, infection, short- or long-term pain, and injury to the bladder or other pelvic organs by the instruments used to place the sling. Ask your surgeon for a complete list of warnings, precautions and possible adverse events.
